Once they are pain free, Total Hip Arthroplasty (THA) patients want to get back to their pre-surgery activities as fast as possible. When compared to national averages, patients treated with the SuperPath® Hip Technique have stayed in the hospital for a shorter amount of time, been discharged to their home more often, and are less likely to return within 30 days for any reason, all without the typical post operative hip restrictions associated with traditional THA techniques.19-21
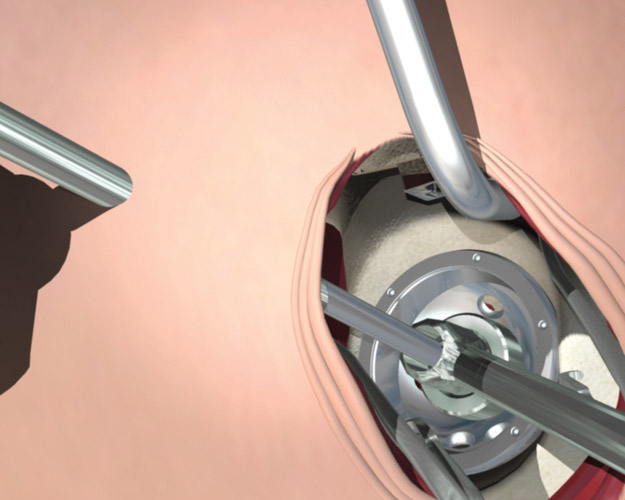
There are many elements to a rapid recovery, and one of the key factors is the choice of surgical approach. Minimally invasive surgical approaches work towards this goal by preserving more muscular structures. By keeping more structures intact, postoperative reduction in pain medication, faster return home from surgery, and faster functional recovery are all possible.
SuperPath® hip approach vs. traditional posterior and anterior approaches
Although the SuperPath® hip technique and the anterior approach are both soft-tissue sparing techniques, a comparison of peer reviewed clinical data from the two approaches illuminates many key advantages of the SuperPath® hip technique:
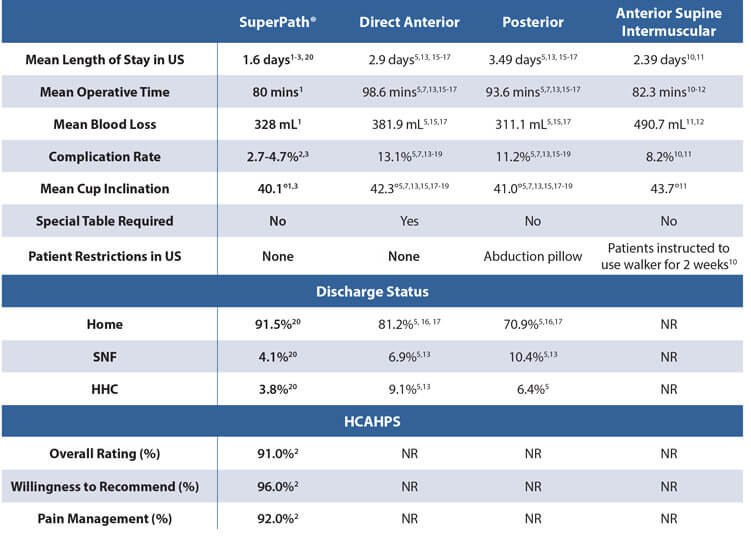
NR: Not Reported; SNF: Skilled Nursing Facility; HHC: Home Health Care
Every patient is different, and individual results will vary. There are risks and recovery times associated with surgery.
PRECAUTIONS & DISCLAIMERS
Every patient is different, and individual results will vary. There are risks and recovery times associated with surgery.
These surgeons are paid consultants for MicroPort Orthopedics. The opinions expressed are theirs alone and do not necessarily reflect the opinions of MicroPort Orthopedics Inc.